Blog
Apr 12, 2024, 5:10 PM
A recent CDC report is raising concern about teens and their mental health, saying rising levels of depression and anxiety are why they’re turning to substances like alcohol and drugs.
Apr 12, 2024, 3:44 PM
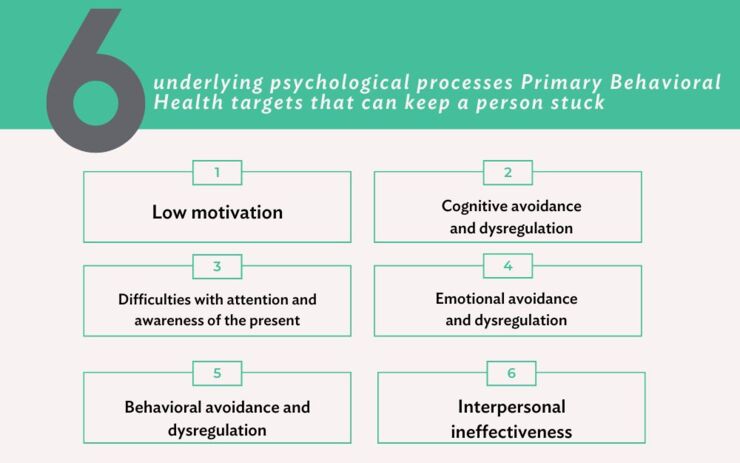
As a leader and innovator in mental health and addiction care for more than a century, Rogers Behavioral Health is using a cutting-edge, evidence-based treatment approach to help reach a broader range of people.
Apr 5, 2024, 12:51 PM
Rogers offers specialized IOP, intensive outpatient programs, and PHP, partial hospitalization programs. These programs are for people who need more treatment than traditional outpatient therapy. In IOP and PHP, a person spends a lot more time in a…
Mar 29, 2024, 11:44 AM
Rogers experts discuss healthy ways to manage stress and how that improves our overall mental and physical well-being.
Mar 22, 2024, 4:09 PM
The outward signs of obsessive-compulsive disorder (OCD) can be easy to see – excessive handwashing, compulsive arranging – behaviors often done in an attempt to address unwanted thoughts. But researchers say focusing on the unseen reason for…
Mar 22, 2024, 3:04 PM
Rogers' Amy Bork, RD, registered dietitian, discusses the impact nutrition can have on mental health.